Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Uvular Necrosis from a Traumatic Bronchoscopy
*Corresponding author: Katrynna Navarro, Department of Internal Medicine Larkin Community Hospital 7031 SW 62nd Avenue South Miami, USA.
Received: March 07, 2022; Published:March 22, 2022
DOI: 10.34297/AJBSR.2022.15.002168
Abstract
Introduction: Uvular Necrosis is a relatively rare and unfortunate circumstance following a traumatic oropharyngeal insertion of medical instruments. These medical instruments cause compression of the uvula decreasing vascular supply leading to necrosis and subsequently sloughing off of the affected area.
Case Presentation: Patient was a 29-year-old cruise ship worker with no past medical history who presented with history of night sweats, fevers, productive cough, anorexia, and weight loss. While the patient was isolated and being worked up for Tuberculosis, patient was scheduled for a bronchoscopy with a bronchioalveolar lavage to rule out intrabronchial lesions and to collect sputum cultures for mycobacterium species. Post-procedure patient experienced sore throat, odynophagia, dysphagia; which was diagnosed as uvular necrosis.
Conclusion: Uvular necrosis is more commonly reported during nasopharyngeal endoscopies and traumatic blind intubations but are rarely associated with bronchoscopies. Though the inciting event is unclear on this patient on whether it was the BAL or the bronchoscope itself, the uvular necrosis was of certainty. With appropriate management, the patient’s symptoms started resolving and the area of necrosis has diminished.
Abbreviations: CXR: Chest X-ray; CT: Computed Tomography; IV: Intravenous; AFB: Acid-Fast Bacillus smear; BAL: Broncheoalveolar Lavage; PCR: polymerase chain reaction.
Introduction
Uvular necrosis is a rare circumstance from endoscopies, forceful suctioning, intubations and bronchoscopies. Though the pathophysiology is the same the inciting trauma may differ. This adverse effect is due to compression of the uvula; obstructing the blood flow causing necrosis and eventual sloughing. Though this occurs in very few patients it is important to note that many experiences symptoms of odynophagia, dysphagia, sore throat; but it can lead to life threatening oropharyngeal edema due to the inflammatory nature. This case study entails the occurrence of this phenomenon secondary to a bronchoscopy and bronchioalveolar lavage to rule out Tuberculosis.
Case Presentation
Patient is a 29 y/o M cruise ship worker who presented to the hospital with a dry cough for 810days with associated fever, chills, night sweats, anorexia, weight loss. He reports cough which was productive initially and was treated with cough suppressants and antibiotics which helped resolve the sputum production. He stated that the fevers have been occurring only at night with temperate reaching a maximum 101*F. In addition, he reported fatigue, multiple joint pain, muscle aches. Patient denied any mosquito or tick bites, but reported travel to Europe, Spain, Panama and Miami. He recalled getting all appropriate vaccinations prior to being employed. He complained of ear fullness and mild rhinorrhea along with a history of exposure to sick contacts on the cruise ship.
On Imaging CXR (Figure 1) showed a patchy opacity of the right apical lung which warranted further examination with a CT. CT (Figure 2) further highlighted the opacity and showed apical reticulonodular consolidations concerning for mycobacterium species. Patient was scheduled to undergo a bronchoscopy with BAL for sputum cultures and for visualization of any endobronchial lesions.

Figure 1: CXR 1/24/20 1. Patchy opacities of the right apical lung which, when correlated with CT of the chest from the same day, may represent an infectious process including mycobacterium avium or tuberculosis. Correlate clinically.
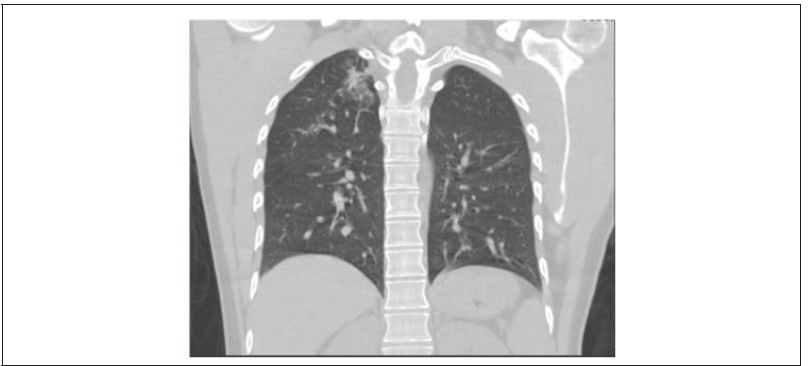
Figure 2: CT Chest 1/24/20 1. Right apical reticulonodular consolidations. May represent developing infectious process including mycobacterium avium or tuberculosis. Recommend clinical correlation.
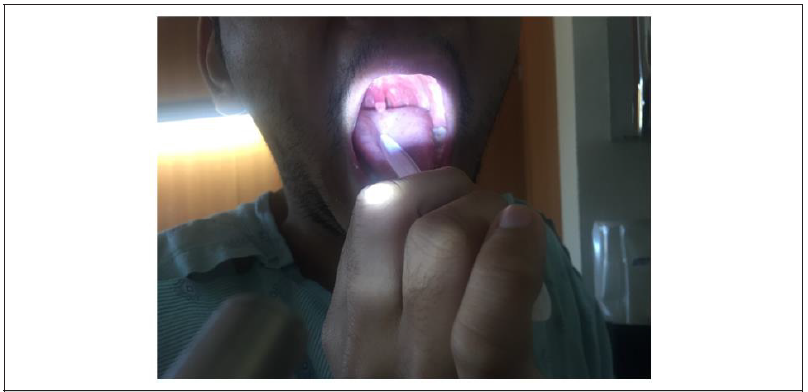
During the bronchoscopy the patient was placed under general anesthesia with Propofol. The patient tolerated the procedure well with stable vital signs and no signs of distress. Twenty-four hours after procedure, patient started complaining of discomfort in his throat along with dysphagia to both solids and liquids and intolerance to both hot and cold liquids. Upon orophyrangeal examination; an erythematous swollen and an elongated uvula was present with an exudative distal tip freely hanging (Figure 3). Patient reported that the uvula would irritate the back of the throat when he laid back or tried to swallow. The remainder of the orophyrngeal exam was unremarkable hence leading towards the diagnosis of uvular necrosis.
Infectious Disease was consulted, and patient was started on Magic mouthwash. Unasyn 3gm IV Q6 hours was initiated due to BAL showing Gram positive cocci in chains and pairs, which was later discontinued due to growth of normal endogenous flora. Six days after the bronchoscopy, patient started feeling some relief and was able to tolerate a soft diet. Upon examination it was noted that the uvula has decreased in size as it was no longer freely moving around and resting on the tongue. The necrotic tip measured to be 1mmx1mm. Once patient’s AFB smears, BAL cultures, PCR results all came back inconclusive, patient was discharged with magic mouthwash and a follow up appointment with an ENT.
Discussion
Uvular Necrosis is a rare adverse effect after trauma most commonly seen by blind intubations, traumatic endoscopies and less commonly through bronchoscopies. Trauma to the soft palate during these procedures can occur in the soft palate, posterior part of the tongue, posterior pharyngeal wall or the uvula. It is common for patients to have a sore throat, dysphagia and pain following a bronchoscopy [1]. They might also report a foreign body sensation which leads to anxiety and disturbed sleep. These symptoms may present for several hours to days and are selfresolving [2]. Some patients may experience life threatening oropharyngeal edema and such patients should be closely monitored post procedure to prevent mortality.
With non-resolving sore throat and dysphagia, the patient’s uvula was predisposed to necrosis which at a later time would slough off [3]. We speculated two different causes for this trauma. The first was thought to be trauma of the uvula by compression against the posterior oropharynx as the patient was supine. The decreased vascular supply for the 15min procedure would have been enough to cause this because it is only supplied by the lesser palatine artery; a branch of the ascending palatine artery [4]. Our second proposed mechanism was due to forceful suctioning during the bronchioalveolar lavage (BAL). Experimentally, it was showing that the vacuum pressures of -500mm Hg are capable of suctioning the uvula [5]. Though the inciting trauma differs from the two, the underlying pathology would still remain as decreased vascular supply.
Amongst the differentials, sore throat from Streptococcus pyogenes was a differential. Group A Strep is the number one bacterial organism to cause tonsillopharyngitis in adults and children with symptoms of sore throat and dysphagia5. Mainstay of treatment for such patients is Penicillin’s and symptomatic care of cough with anti-tussive and oral analgesia [6]. Our patient received Unasyn (Ampicillin/Sulbactam) along with Magic Mouthwash (diphenhydramine, viscous lidocaine, antacid, nystatin, and corticosteroids).
Conclusion
Though there are many mechanisms of uvular trauma our patient was introduced to this either through traumatic insertion of bronchoscope or vigorous suctioning during the BAL. The patient experienced telltale symptoms such as sore throat, odynophagia, dysphagia and foreign body sensation. Despite different inciting events the pathophysiology remains the same between all traumas; decreased vascular supply for a short period of time described as short as 15 minutes as in this case. Uvular Necrosis should be of concern to the provider as life threatening oropharyngeal edema can be a sequalae of this event.
Consent
A written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editorin- Chief of this journal.
Availability of Data and Materials
The supporting data and materials of this case report are available upon request to the corresponding author.
Competing Interests
All authors in this case report declare that they have no competing interest.
Authors’ contributions
All authors participated in the management of this patient, conceived the idea of the case report and participated in the drafting of the study.
Acknowledgement
George J Michel MD, FACP for his amazing teaching that lead to the conceptualization of this case report and the patient for consenting to allow us to publish this report.
References
- Elise Orvedal Leiten, Einar Marius Hjellestad Martinsen, Per Sigvald Bakke, Tomas Mikal Lind Eagan, Rune Grønseth (2016) Complications and Discomfort Of Bronchoscopy: a Systematic Review Eur Clin Respir J 3: 33324.
- P M Suratt, J F Smiddy, B Gruber (1976) Deaths and complications associated with fiberoptic bronchoscopy. Chest 69(6): 747-751.
- Atkinson CJ, Rangasami J (2006) Uvula necrosis: an unusual cause of severe post-operative sore throat. Br J Anesthesia 97(3): 426-427.
- Jae Hoon Cho, Jin Won Kim, Hyoung Woo Park, Jeffrey D Suh, Jin Kook Kim (2017) Arterial supply of the human soft palate. Surg Radiol Anat 39(7): 731-734.
- M S Bogetz, B J Tupper, A C Vigil (1991) Too much of a good thing: uvular trauma caused by overzealous suctioning. Anesthesia and Analgesia 72(1): 125-126.
- https://www.uptodate.com/contents/treatment-and-prevention-of-streptococcalpharyngitis?search=streptococcus%20pyogenes&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.